Plantar Fasciitis
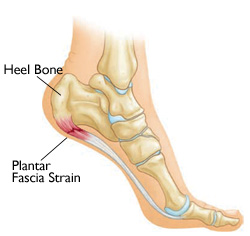 Plantar fasciitis is inflammation of the thick tissue on the bottom of the foot. This tissue is called the plantar fascia, and it connects the heel bone to the toes and creates the arch of the foot.
Plantar fasciitis is inflammation of the thick tissue on the bottom of the foot. This tissue is called the plantar fascia, and it connects the heel bone to the toes and creates the arch of the foot.
Plantar Fasciitis Causes, Incidence, and Risk Factors
Plantar fasciitis occurs when the thick band of tissue on the bottom of the foot is overstretched or overused. The fascia may swell, and its tiny fibers may begin to fray. This can be painful and make walking more difficult. You are more likely to get plantar fasciitis if you have:
- Foot arch problems (both flat feet and high arches).
- Poor foot mechanics.
- Tight Achilles tendon (the tendon connecting the calf muscles to the heel).
- Shoes with poor arch support or soft soles.
Plantar fasciitis is commonly thought of as being caused by a heel spur, but research has found that this is not the case. On x-ray, heel spurs are seen in people with and without plantar fasciitis. The heel spur can form in response to the plantar fascia's tug on the heel bone.
Plantar Fasciitis Symptoms
The most common complaint is pain and stiffness in the bottom of the heel. The heel pain may be dull or sharp. The bottom of the foot may also ache or burn. The pain is usually worse:
- In the morning when you take your first steps.
- After standing or sitting for a while.
- When climbing stairs.
- After intense activity.
The pain may develop slowly over time, or suddenly after intense activity.
Signs & Tests
The health care provider will perform a physical exam. This may show:
- Tenderness on the bottom of your foot.
- Flat feet or high arches.
- Mild foot swelling or redness.
- Stiffness or tightness of the arch in the bottom of your foot.
X-rays may be taken to rule out other problems.
Plantar Fasciitis Treatment
Your health care provider will usually first recommend:
- Oral and topical medications to reduce pain and inflammation.
- Heel and foot stretching exercises.
- Night splints to wear while sleeping to stretch the foot.
- Resting as much as possible for at least a week.
- Wearing shoes with good support and cushions.
- Orthotics to help support the mechanics of your foot.
- Steroid injections to decrease inflamation.
Other steps to relieve pain include:
- Ice application to the painful area. Do this at least twice a day for 10 - 15 minutes, more often in the first couple of days.
- Limiting barefoot walking.
If these treatments do not work, your health care provider may recommend:
- Wearing a walking cast for 3-6 weeks. It can be removed for bathing.
- Custom-made shoe inserts (orthotics).
Non-surgical treatments almost always improve the pain, but sometimes surgery is needed. Treatment can last from several months to two years before symptoms get better. Most patients feel better in nine months. Some people will need surgery, during which the fascia is partially cut to release tension.







